WEIGHT LOSS & WELLNESS
Female Bioidentical Hormone Replacement
Female Bio-Identical Hormone Replacement Therapy (BHRT) in Texas involves the use of hormones that are structurally identical to the hormones naturally produced by a woman’s body. Natural Hormones are essential to healthy, vigorous and more youthful bodily function.
Female Bioidentical Hormone Replacement: Concierge care by experienced Board Certified Nurse Practitioners.


Bio-Identical Hormone Replacement Therapy at Aesthetics Concierge of Texas
What is included in the treatment package:
– Consultation with one of our experts for personalized discussion
– Lab work to understand the intricacies of your unique needs, paving the way for a tailored hormone replacement plan
– Follow up consultation for comprehensive monitoring
🚨 Superbill for insurance submission 🚨
Ready To Book An Appointment?
Ready to schedule your Initial Consultation with our Nurse Practitioners? Click on the link below!
Learn More About Female Bio-Identical Hormone Replacement Therapy
FEMALE HORMONES
Learn more about Female BHRT from our Partner Dr. Jim Hrncir.
HORMONES AND LIBIDO
Learn more about how Female BHRT affects libido from our partner Dr. Jim Hrncir.
Learn More About Hormone Replacement?
Female Bio-Identical Hormone Replacement Therapy (BHRT) involves the use of hormones that are structurally identical to the hormones naturally produced by a woman’s body. Natural Hormones are essential to healthy, vigorous and more youthful bodily function.
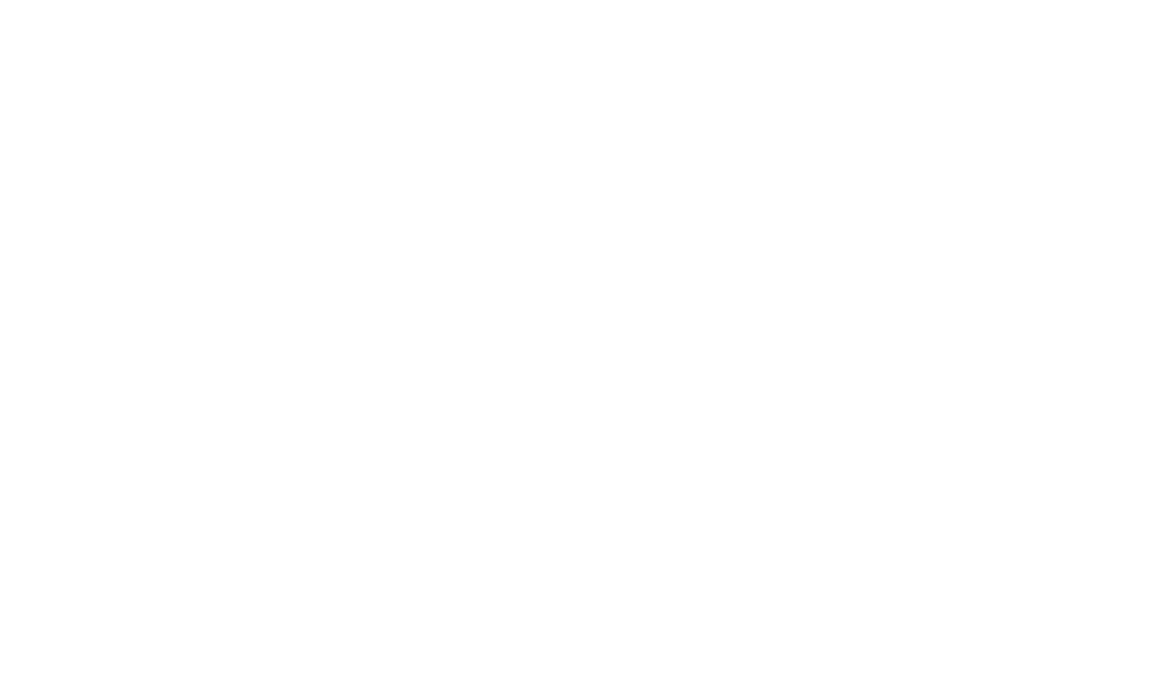
For optimal wellness, men and women must maintain a proper balance of the natural hormones:
- Estrogen
- Progesterone
- Testosterone
- DHEA
- Pregnenolone
- Cortisol
- Thyroid
These natural hormones are derived from plant sources, usually soy or yam, and then modified to become chemically identical to human hormones. Because they are exactly what the human body produces, we refer to these hormones as biologically identical or “Bio-Identical” for short. These “prescription-only” hormones are then used to replace missing or depleted levels in the body.
“Bio-identical” hormones, naturally occurring in the human body, cannot be patented by drug companies and are therefore largely supplied by compounding pharmacies.
Ready To Book An Appointment?
Ready to schedule your Initial Consultation with our Nurse Practitioners? Click on the link below!
Types of Female Bio-Identical Hormones
Estrogen
Estrogen can alleviate common menopausal symptoms such as hot flashes, night sweats, and vaginal dryness, enhancing overall comfort during this life stage and helps mitigate the bone loss that occurs during menopause, reducing the risk of fractures and osteoporosis.
WHAT ARE THE SIGNS OF ESTROGEN DEFICIENCY?
Estrogen plays a vital role in various physiological functions in women. Signs of estrogen deficiency may include:
Hot flashes
Night sweats
Vaginal dryness
Forgetfulness or mental fogginess
Mood change or recent onset of depression
Difficulty falling asleep
Sagging breasts and loss of breast fullness
Loss of skin radiance or quickly aging skin
Dry eyes
Lessened self image and attention to appearance
Weight gain
Increased joint or muscle pain
Scalp hair loss
Decreasing bladder control
Pain with sexual activity
Decreased sexual drive or sensuality
Increased anxiety
WHAT ARE THE SIGNS OF ESTROGEN EXCESS?
Estrogen levels can be influenced by factors like age, health conditions, and lifestyle. If someone suspects an imbalance, the signs of estrogen excess may include:
Nausea
Increased fluid retention
Uterine fibroids worsening or developmen
Weight gain, especially in hips
Worsening fibrocystic breasts
Increased breast and nipple tenderness
Pelvic cramps with or without bleeding
Headaches/migraines
Progesterone
During the phase of perimenopause, hormonal fluctuations become more pronounced, impacting various aspects of their well-being. Progesterone, a crucial hormone in the female reproductive system, plays a pivotal role in maintaining hormonal balance. Recognizing the signs of pre-menopausal progesterone deficiency is essential for understanding and addressing hormonal imbalances. Often used in combination with estrogen, progesterone helps balance the effects of estrogen and supports the uterine lining. Here are key indicators that may suggest a deficiency in progesterone levels during the pre-menopausal phase:
What are signs of Pre-menopausal progesterone deficiency?
PMS
Heavy and/or frequent periods
Lack of period or amenorrhea
Endometriosis or fibroids
Development of insomnia
Ovarian cysts
Sense of normalcy only during second week of cycle
Fibrocystic breasts
Anxiety, irritability, and nervousness
Spotting a few days before period
Infrequent period
Water retention
What are signs of Menopausal progesterone deficiency?
Insomnia
Anxiety, irritability, and nervousness
Increased hot flashes
Fibrocystic breasts
Water retention
Testosterone
Obtaining optimal female levels of testosterone improves mood, brain function, metabolism, and libido.
Testosterone reduces risks of breast cancer and osteoporosis.
What are signs of testosterone deficiency?
- Decreased sex drive
- Loss of muscle tone or muscle mass
- Indecisiveness
- Decreased memory or foggy brain
- Loss of sense of security
- Lack of energy and stamina
- Decreased exercise tolerance
- Decreased armpit, pubic, or body hair
- Slowed metabolism
What are signs of testosterone excess?
- More irritable
- Agitation and anger
- Scalp hair loss or unwanted hair growth (hirsutism)
- Weight gain
- Acne

Benefits of Female Bio-Identical Hormone Replacement Therapy
- Relief from menopausal symptoms: BHRT is known to alleviate common menopausal symptoms such as hot flashes, night sweats, mood swings, and sleep disturbances
- Bone Health: Estrogen plays a crucial role in maintaining bone density. BHRT may contribute to bone health and reduce the risk of osteoporosis.
- Improved Mood and Mental Health: Hormonal imbalances can impact mood and cognitive function. BHRT aims to restore hormonal equilibrium, potentially improving mental well-being and reducing symptoms of anxiety and depression.
- Enhanced Libido: Hormonal imbalances can affect sexual desire. BHRT may contribute to improved libido and sexual satisfaction.
- Cardiovascular Health: Estrogen has been shown to have a protective effect on the cardiovascular system. BHRT may support heart health in postmenopausal women.
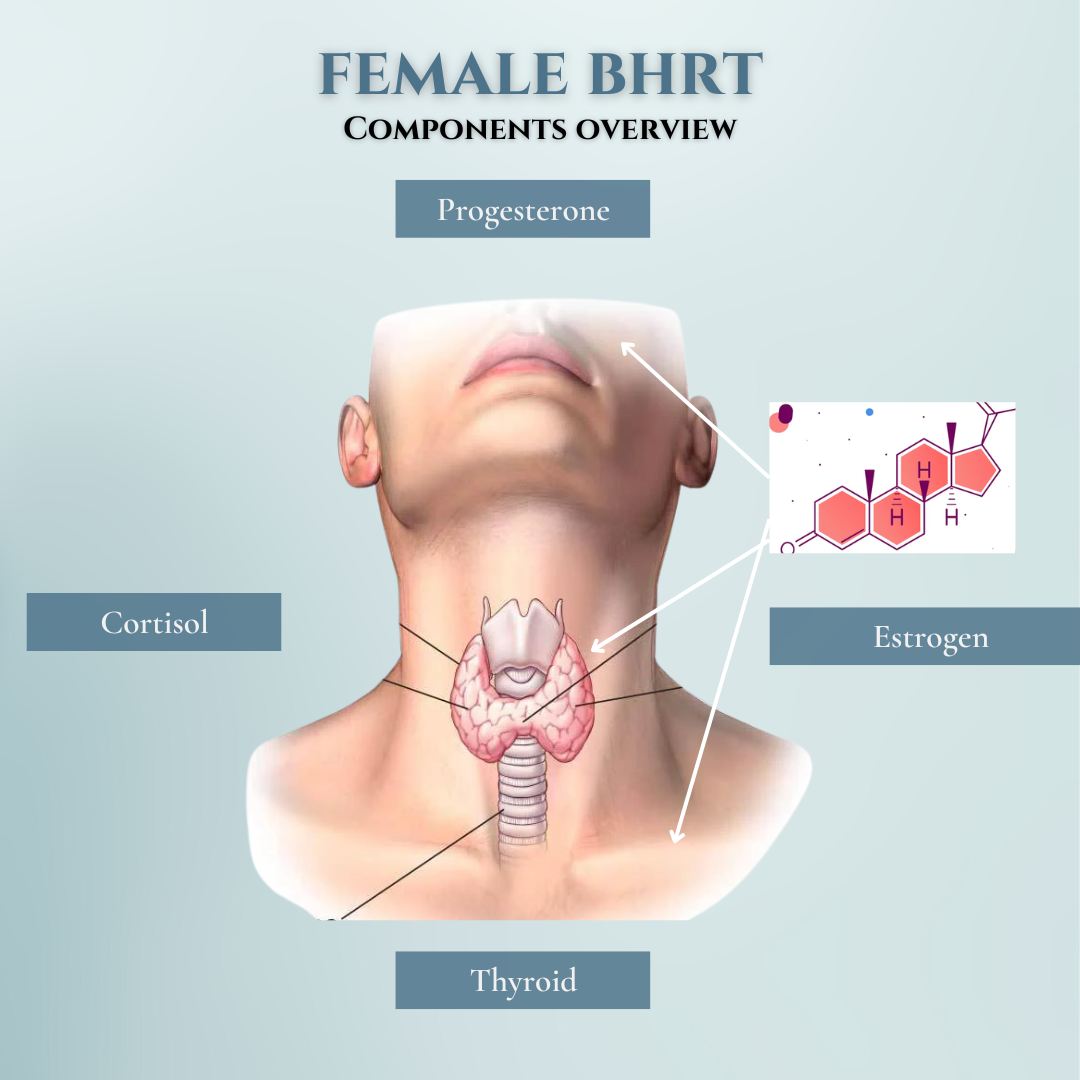
Tips for Breast Cancer Prevention
- Maintain hormone balance before and after menopause (use bioidentical hormones)
- Discontinue birth control pills (use alternative birth control). Long-term use of oral birth control has been associated with a 20% increased risk of breast cancer (when off the pill for five years, risks return to normal)
- Exercise and Control Weight:
- Cancer-protective estrogen metabolism with exercise
- Hormone balance
- Immune stimulation
- Weight control
- Stress reduction
- East daily serving of cruciferous vegetables and take antioxidants (Vitamin C, CoEnzyme Q10, Glutathione, Resveratrol)
- Take 2-4 grams daily of high-quality fish oil
- Reduce saturated fats, eliminate trans-fats
- Don’t smoke
- Maintain Vitamin D3 levels of 65-100 in serum
Why don’t we use implantable pellets?
Supra-physiologic dosing
Widespread reporting of pt harm
Implantation issues
No control once implanted
Risk of scar tissue and dermatitis
ALL ABOUT THE THYROID
T4 is the precursor thyroid hormone; HPT axis feedback from T4 levels (increased TSH when low).
T3 is the active thyroid hormone.
Symptoms of low thyroid
Fatigue
Weight gain
Loss of the outer half of eyebrows and unexpected scalp hair loss
Body temperature below 98.2
Cold hands and feet, intolerance to cold
Dry skin, weak or ridged nails
Decreased memory and concentration
Puffy eyes and swollen eyelids
Low blood pressure
Depressed mood
Muscle weakness
Headache
Fluid retention
Symptoms of high thyroid
Tachycardia
Heart palpitations
Nervousness/anxiety
Insomnia
Weight loss
Subclinical hypothyroidism
- Subclinical hypothyroidism associated with a 260% increase in the prevalence of heart disease, atherosclerosis, low metabolism, weight gain, increased auto immune diseases, more inflammatory and chronic pain, increased glandular cancers and cancer mortality
Reverse T-3:
- Competitor for thyroid binding sites, blocks actions of T-3, commonly observed in patients with hashimotio’s, chronic stress, severe caloric restriction, iron deficiency, chronic illness
- Can consider selenium for reduced conversion of T4 to reverse T3 (***ONLY 200 mcg/day)
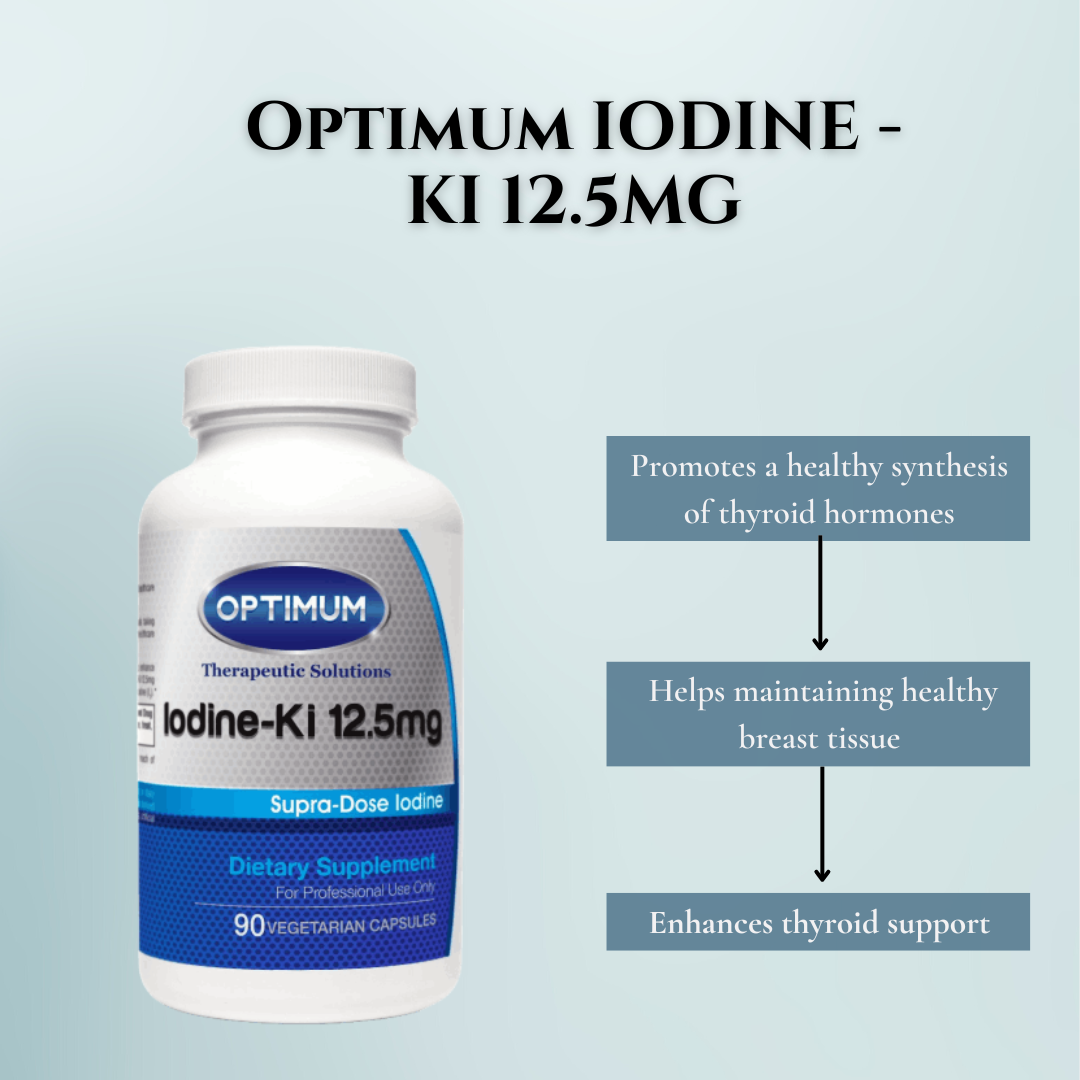
Iodine and the Thyroid gland:
- Iodine is an essential ingredient in the thyroid hormones
- Estimate 90% of Americans are iodine deficient
- Consider supplementation with Optimum Iodine Ki 12.5mg 3 times per week (https://www.optimumtherapeuticsolutions.com/?code=AestheticsConTX)
Supplements helpful to consider for thyroid health:
- (https://www.optimumtherapeuticsolutions.com/?code=AestheticsConTX
- Optimum ThyroPromote OTS 1 cap q am
- Optimum Iodine Ki 12.5mg 3 times per week
- Zinc 50mg/day
- Chelated iron 30-100mg/day
Why do we recommend Desiccated Thyroid vs. Synthroid/Levothryroxine
Synthroid is a brand name for levothyroxine, a synthetic (man-made) form of the thyroid hormone thyroxine, or T4. NP Thyroid, Armour Thyroid, and W.P Thyroid are brand names for a natural form of thyroid hormone. It is made from the dried thyroid glands of pigs. More than
15% of hypothyroid patients with a normal TSH on Levothyroxine feel hypothyroid. This happens less with patients on desiccated thyroid.
In studies comparing desiccated thyroid with Levothyroxine, patients on desiccated thyroid preferred desiccated thyroid over Levothyroxine.
Levothyroxine contains only T4, while T3 is the active hormone. The body makes 85% T4 and 15% T3. Conventional endocrinologists hope the body goes into over-drive to convert the T4 to T3, but in many patients that doesn’t happen.
Rules when you have your labs drawn:
In AM, fasting
If receiving transdermal, do not apply hormones with hand or to arm of blood draw for 3 days prior to lab draw
Transdermal: draw 24 h after last application
Sub-Q: draw AM of day 3-4 (before next injection)
No Biotin for more than 3 days prior to draw
NO AM meds until after lab draw (including thyroid medication …wait to take all meds until after draw)
Our Partnership with Las Colinas Pharmacy for Exceptional Care and Personalized Medications
Re-Gen & Aesthetics Concierge of Texas is a partner of Las Colinas Pharmacy. After the consultation takes place, we send your prescription to the Las Colinas Pharmacy and they will ship you the medication within one week.
Established in 1984, Las Colinas Pharmacy is recognized for providing the highest level of service, whether dispensing traditional prescription drugs or personalized, compounded medications.
One of the original pioneers in pharmacy compounding, Las Colinas Pharmacy sustains cutting edge knowledge, technology and quality control procedures. LCP is proud to claim accreditation by PCAB (Pharmacy Compounding Accreditation Board).
LCP’s pharmacist founder, Jim Hrncir, received national attention when he appeared on several episodes of the Dr. Phil Show. Jim worked with Dr. Phil’s wife, Robin McGraw to achieve hormone balance. He is also featured in her book, What’s Age Got to Do with It?: Living Your Healthiest and Happiest Life. Hrncir says experts in the field refer to a large number of studies which suggest the balanced use of natural hormones help patients feel better and possibly lower the risk of heart disease, osteoporosis, and cancer.
At Aesthetics Concierge of Texas, we partner with Las Colinas Pharmacy to deliver exceptional care and quality prescriptions.


Female Bioidentical Hormone Replacement FAQ
In this FAQ section, we will answer some common questions about Female BioIdentical Hormone replacement. Whether you’re considering this treatment or just curious about the procedure, this section will provide you with valuable information to help you make an informed decision.
Please reach us at [email protected] if you cannot find an answer to your question.
What is the goal of bioidentical hormones replacement?
The goal of BHRT is maintain optimal physiologic levels in order to improve quality of life. Note: we do NOT replace hormones to supra-physiologic levels.
How do I know if I need Female Bio-Identical Hormone Therapy (BHRT)?
BHRT may be considered if you are experiencing symptoms of hormonal imbalance, such as hot flashes, mood swings, fatigue, and changes in libido. Consultation with a healthcare provider, including hormone level testing, can help determine if BHRT is suitable for your individual needs.
Is the BHRT procedure considered safe?
Bio-Identical Hormones are derived from plant sources and designed to replicate the molecular structure of hormones naturally produced by the body. When prescribed and monitored by qualified healthcare professionals, BHRT is generally considered safe. It’s crucial to discuss your health history, concerns, and undergo regular monitoring during treatment.
Are there risks with taking bioidentical hormones?
Based on extensive clinical data and studies over many years compared to placebo, there is NO evidence that hormones cause increased risk of
Breast cancer
Heart disease
Stroke
Colorectal cancer
Hip fracture
Dementia
All cause mortality:
What are the benefits of BHRT?
BHRT is known for effectively addressing symptoms related to hormonal fluctuations, including hot flashes, night sweats, irritability, insomnia, and reduced libido. Additionally, BHRT may contribute to improved energy levels, mood stability, and overall well-being during various life stages.
Ready To Book An Appointment?
Ready to schedule your Initial Consultation with our Nurse Practitioners? Click on the link below!
